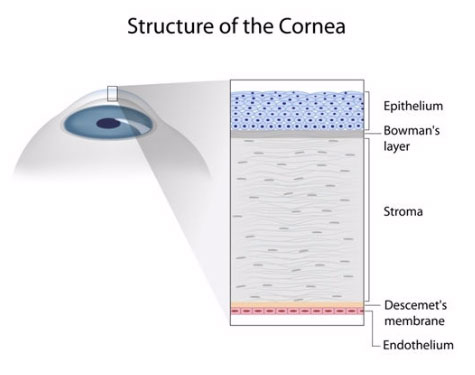
The cornea is the clear window at the front of the eye which focuses all the light entering the eye. Abnormalities of the cornea may cause a change to the shape of the cornea or make it become cloudy. These abnormalities both make the vision blurred.
Common conditions affecting the cornea are Keratoconus, Fuch’s Endothelial Dystrophy and viral or bacterial infections.
When the cornea cannot be cleared by medical therapy, a corneal transplant may be required.
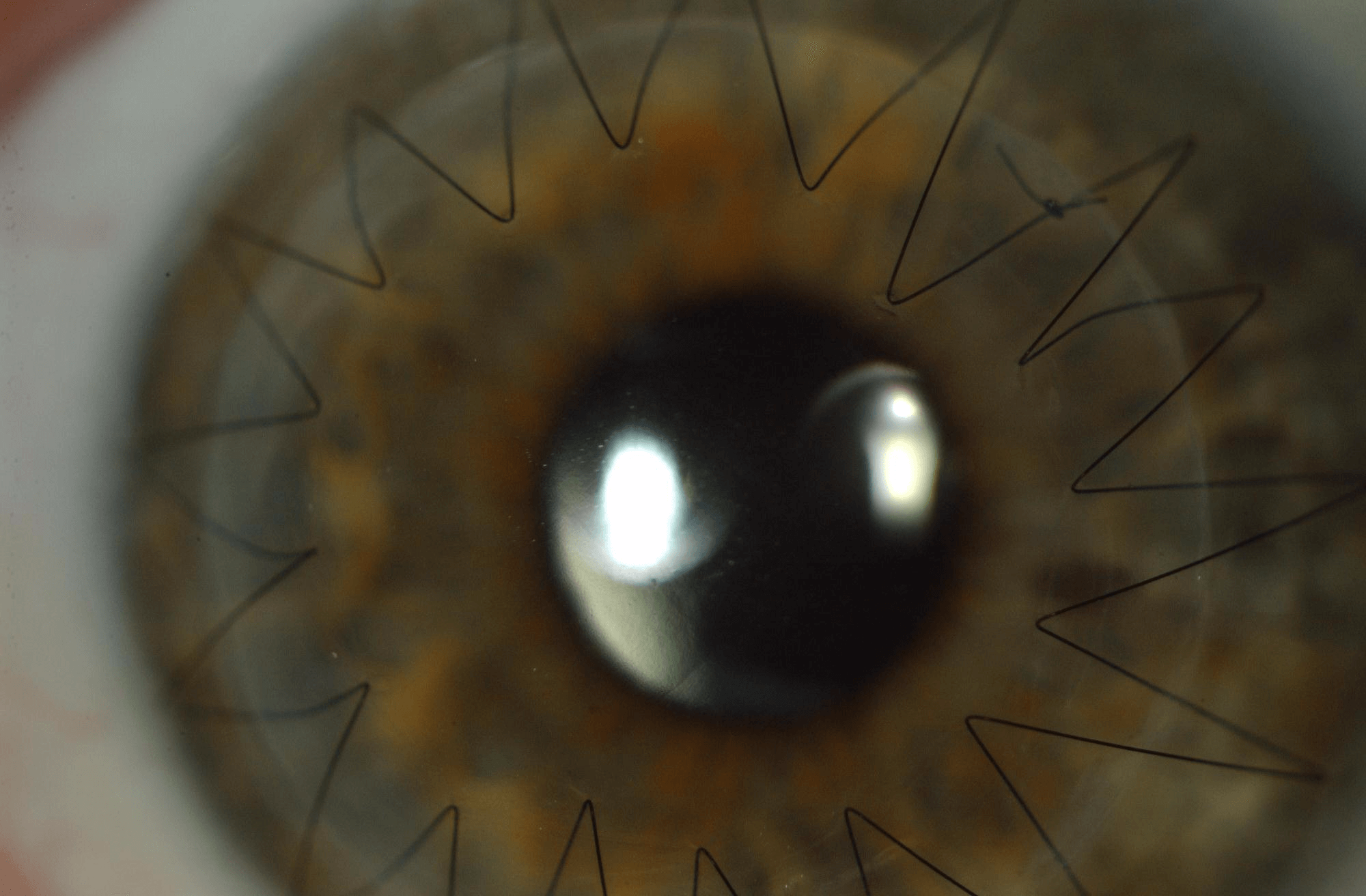
Corneal Graft
There are two ways of performing this surgery-
- Partial thickness corneal graft (Deep Anterior Lamellar Keratoplasty- DALK) is a modern technique whereby the outer 95% of the cornea is removed and replaced with the outer 2 layers from a donor cornea.
- Full thickness corneal grafts (Penetrating Keratoplasty) replace a central button of all three layers of the cornea.
Possible advantages of partial thickness over full-thickness grafts
- Much lower risk of graft rejection
- Lower risk of intraocular problems such as serious infection or bleeding
- The corneal wound is stronger
Goals of surgery
- Improved vision
- 90% of transplant recipients reach driving standard if the eye is otherwise healthy
- But may need glasses, contact lenses or sometimes further laser surgery for best results.
- It may take up to 18 months until the full improvement in vision is appreciated
- Most patients have a reduced need for contact lenses or glasses
DMEK
Why do you need a corneal transplant?
The cornea is the clear spherical dome on the front of the eye. The cells on the inside of the cornea (endothelial cells) maintain corneal clarity and quality of vision. They can become dysfunctional for a variety reasons including genetics (Fuch’s endothelial dystrophy), previous eye surgery (pseudophakic or aphakic bullous keratopathy) or rejection of a previous corneal graft.
Endothelial keratoplasty is a modern technique to replace the dysfunctional cells with the same cell layer from a donor cornea.
DMEK (Descemet membrane endothelial keratoplasty) surgery is the most advanced form of this surgery and transplants only the essential cells and a thin supporting membrane.
Goals of surgery
- Improve vision
- A small number of patients may have this procedure to reduce pain
Advantages of DMEK surgery
- Greater improvement in vision
- Better quality of vision
- Quicker recovery
- Less chance of rejection
- Minimal stitches
Risks of Endothelial Keratoplasty Rare but serious complications
- light-threatening infection inside the eye (1 in 1000)
- Severe haemorrhage causing loss of vision
- Retinal detachment
- Acute glaucoma causing loss of vision
Corneal transplant rejection
A corneal transplant can be identified and attacked by the patient’s immune system. This happens in only 1 in 30 patients in the first 2 years after transplantation but can cause graft failure. It is important to recognize the symptoms of rejection early so anti-rejection medication can be started as soon as possible.
Symptoms of rejection are:
- Red eye
- Sensitivity to light
- Reduced vision
- Mild pain
If you experience any of these symptoms you should contact Dr Green’s clinic immediately.
Graft Failure
When a graft fails the cornea becomes cloudy again and vision becomes blurred.
Glaucoma
Chronic mild glaucoma occurs in a small number of patients (approximately 4%). It is usually controlled by eyedrops but occasionally requires surgery.
Graft detachment
Partial detachment of DMEK grafts occurs in approximately 30% of cases and these patients need to have a second injection of air.
Complete detachment occurs in approximately 10% of patients and this is generally repaired in theatre with a repeat corneal graft.
The operation
The operation is day surgery performed under local anaesthetic and takes about one hour. Some patients need a cataract operation at the same time. Through a small incision the patients’ endothelium is removed and a thin sheet of donor endothelium is inserted and floated into position with a bubble of gas, which will remain present for a week.
Normal experiences after the operation
- You will need to lie flat for 1 hour after the operation.
- Its very important that you don’t fly in an aeroplane after the operation until the gas bubble is completely gone and this is confirmed by your doctor; this is usually two weeks
- Here will be a gradual improvement in vision over 4 weeks
- Mild amount of ocular discomfort and visible bleeding around the eye
- You will be examined by Dr Green after the surgery and can go home the same day.
- You will be seen a few days after the operation and again a week later to make sure the graft stays in position.
- You will have about 6 visits to the outpatient clinic in the first year.
- We generally recommend that you take 2 weeks off work – discuss your case with your doctor.
- You will need to use anti-rejection eyedrops for at least 6 months and in some cases indefinitely.